When your body faces injury or infection, it initiates acute inflammation, which quickly involves blood vessel dilation, immune cell recruitment, and rapid clearance of threats, resolving within days or weeks. If the inflammation fails to resolve, it can turn chronic, characterized by ongoing immune activity, tissue damage, and infiltration of different immune cells like lymphocytes. Understanding these mechanisms helps you grasp how inflammation can either heal swiftly or persist silently, impacting your health over time.
Key Takeaways
- Acute inflammation is a rapid, short-term response involving neutrophils, aiming to contain threats and promote healing.
- Chronic inflammation persists over months or years, involving lymphocytes and macrophages, leading to ongoing tissue damage.
- Resolution of acute inflammation restores tissue function, whereas failure to resolve causes transition to chronic inflammation.
- Key features of acute inflammation include redness, heat, swelling, pain, and loss of function, while chronic inflammation causes subtle, long-term damage.
- Transition from acute to chronic inflammation occurs when the initial response fails to eliminate the threat or resolve tissue injury.
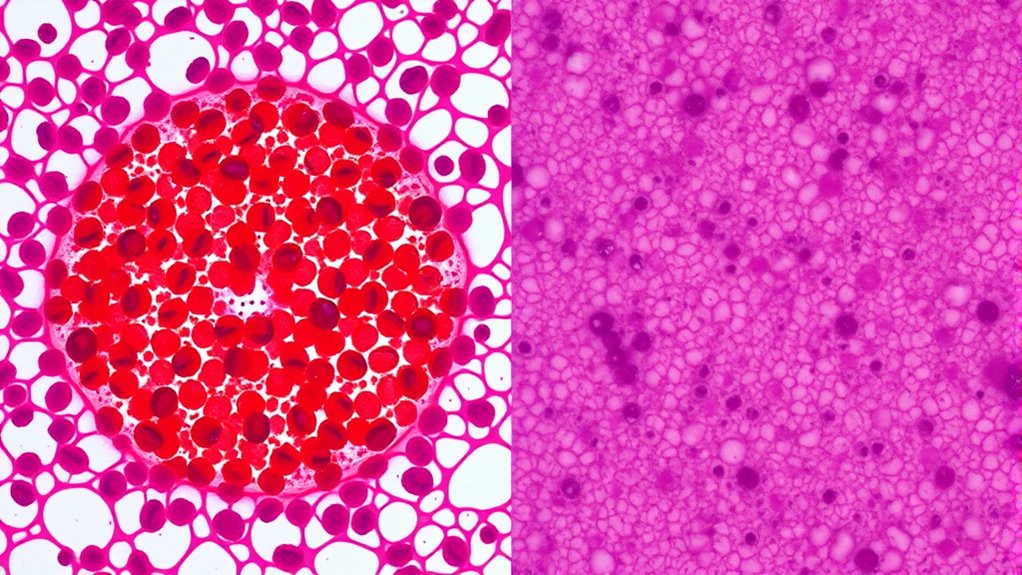
Have you ever wondered what sets acute inflammation apart from chronic inflammation? The answer lies in how your body responds to injury or infection. When tissue damage occurs—whether from a cut, infection, or irritation—your immune system springs into action. In acute inflammation, this immune response is swift and targeted. Blood vessels dilate to increase blood flow, bringing immune cells like neutrophils and macrophages to the site of injury. These cells work quickly to neutralize pathogens and clear out dead or damaged tissue. The process is designed to be short-lived, usually resolving within days or weeks, allowing your tissue to heal properly. The hallmark of acute inflammation is its rapid onset and clear signs: redness, swelling, heat, pain, and sometimes loss of function. It’s your body’s immediate effort to contain the threat, repair the damage, and restore normal function. Additionally, prompt diagnosis and treatment can help prevent the transition from acute to chronic inflammation.
In contrast, chronic inflammation develops when this immune response lingers or becomes dysregulated. Instead of resolving, the ongoing immune activity can cause continuous tissue damage, even in the absence of an ongoing threat. Your immune system keeps releasing inflammatory mediators and recruiting immune cells, which may inadvertently attack healthy tissue. This persistent response can result from unresolved infections, autoimmune conditions, or prolonged exposure to irritants. Unlike the quick, organized reaction seen in acute inflammation, chronic inflammation is more insidious, often developing over months or years. It can lead to significant tissue damage, scarring, and loss of function, which makes it more hazardous in the long run. The immune response in chronic inflammation tends to involve different types of immune cells, such as lymphocytes and plasma cells, which sustain the inflammatory process. These cells release cytokines and enzymes that perpetuate tissue destruction. Because of its prolonged nature, chronic inflammation often causes subtle but ongoing damage, making it harder to detect and treat effectively.
Understanding the differences between acute and chronic inflammation helps you grasp how your body tries to heal itself. Acute inflammation is a necessary, protective response that promotes healing and fights infection, with tissue damage being limited and repair swift. Conversely, if the immune response becomes chronic, the ongoing tissue damage can lead to various diseases like arthritis, inflammatory bowel disease, or even cardiovascular problems. Recognizing these distinctions emphasizes the importance of controlling inflammation early on, to prevent minor injuries from escalating into persistent, damaging conditions. Your immune response is crucial, but when it’s misregulated or prolonged, it can turn against your own tissues, highlighting the fine line between healing and harm.
Frequently Asked Questions
How Can Inflammation Be Effectively Diagnosed in Clinical Settings?
To effectively diagnose inflammation in clinical settings, you should consider biomarker identification like C-reactive protein and erythrocyte sedimentation rate. Additionally, imaging techniques such as MRI or ultrasound help visualize inflammation and its location. Combining these approaches allows for accurate assessment of the inflammatory process, helping you determine its severity and duration, and guiding appropriate treatment strategies. Always interpret results within the broader clinical context for best outcomes.
What Lifestyle Factors Influence the Transition From Acute to Chronic Inflammation?
You can influence the shift from acute to chronic inflammation through your lifestyle choices. Poor dietary habits, such as high sugar and processed food intake, promote sustained inflammation. Additionally, inadequate stress management keeps your body in a constant state of stress, which hampers your immune response and fosters chronic inflammation. By improving your diet and practicing stress reduction techniques, you help prevent inflammation from becoming long-lasting and damaging.
Are There Genetic Predispositions to Developing Chronic Inflammation?
Ever wonder if your genes make you more prone to chronic inflammation? Genetic susceptibility plays a significant role, as variations in inflammatory genes can influence how your body responds to injury or infection. These genetic differences may increase your risk for persistent inflammation, which can lead to chronic health issues. While lifestyle impacts are essential, understanding your genetic makeup helps you better manage and prevent long-term inflammatory conditions.
How Do Anti-Inflammatory Medications Differ in Targeting Acute Versus Chronic Inflammation?
You might wonder how anti-inflammatory medications differ in targeting acute versus chronic inflammation. These drugs focus on immune modulation and drug specificity to address distinct inflammatory processes. For acute inflammation, they often quickly reduce pain and swelling by inhibiting prostaglandins. In chronic cases, they more precisely target immune pathways involved in ongoing tissue damage, helping to control persistent inflammation without broadly suppressing the immune system.
What Are Emerging Therapies for Managing Chronic Inflammatory Conditions?
Did you know that chronic inflammatory conditions affect over 10% of the global population? Emerging therapies focus on biologic agents that target specific inflammatory pathways, offering more precise treatment options. Personalized therapies are gaining popularity as they tailor interventions to individual patient profiles, improving outcomes. These innovative approaches aim to reduce side effects and enhance quality of life by addressing the unique mechanisms driving each person’s chronic inflammation.
Conclusion
Understanding the differences between acute and chronic inflammation helps you grasp how your body responds to injury or infection. While acute inflammation is a quick, helpful defense, chronic inflammation can silently cause damage over time. Are you paying attention to the signs your body gives you? Recognizing these mechanisms empowers you to take better care of your health and prevent long-term issues. After all, awareness is the first step toward keeping inflammation in check.









